
Here’s the link to my latest summary review paper in EBD
Surgical Regenerative Treatment of Peri-implantitis

Here’s the link to my latest summary review paper in EBD
 Introduction
Introduction
It has long been established that smoking is a significant modifying factor in the progression of periodontal disease and eventual tooth loss (Dietrich et al. 2015; Zeng et al. 2014). The established treatment of periodontal disease is based on the elimination of pathogens through subgingival scaling and root planing (SRP), if periodontal disease remains following this initial ‘hygienic phase’ then treatment can be repeated with the addition of systemic antibiotics too good effect (Keestra et al. 2014; Rabelo et al. 2015). Thus, the aim of this study is to conduct a systematic review and meta-analysis to evaluate the effectiveness of systemic antibiotic therapy associated with periodontal treatment in smokers.
Methods
This review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement with the focused question; “Do adjunctive antimicrobials improve the clinical outcome of non-surgical therapy (scaling and root planing [SRP]) in the treatment of periodontitis in smokers?”
The following inclusion criteria were applied: Randomized controlled clinical trials; studies published in English; studies with smoker patients (at least 10 cigarettes per day for at least five years) diagnosed with chronic periodontitis; patients without significant systemic diseases ; aged between 30 and 70 years; not receive periodontal treatment in the last six months; used systemic antibiotic therapy associated with periodontal treatment; present the results of the test and control groups, and assessments of clinical periodontal parameters such as probing depth (PD), bleeding on probing (BOP) and clinical attachment level (CA). Exclusion criteria were local antibiotic therapy and trials not published in English.
Two researchers independently selected and screened the articles. Data bases were searched from July 1994 to August 2016. The included databases were MEDLINE, Cochrane Controlled Clinical Trial Register, Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, CINAHL, Science Direct, and ISI Web of Knowledge, Scopus, and manually searched relevant specialist journals. Quality assessment was undertaken using the Jadad scale.
Results
The systematic Search found 3 papers out of 68 which fulfilled the inclusion criteria for meta-analysis. On the JADAD risk of bias assessment only 8/30 studies were evaluated as high quality.
Meta-analysis results (Primary outcomes)
| Mean Difference Probing Depth | (p = 0.0359 MD -0.32, 95% CI -0.50 – -0.14) |
| Mean Difference Clinical Attachment level | (p = 0.0161 MD -0.22, 95% CI -0.39 – -0.06) |
| Mean Difference Bleeding on Probing | (p = 0.446 MD -0.04, 95% CI -0.13– 0.06) |
Author’s Conclusion
“The results of our meta-analysis reveal the clinical benefits of systemic antibiotics as an adjunct to the non-surgical periodontal treatment of smokers. These clinical improvements, although statistically significant, appeared to be of little clinical relevance.”
Comments
In the discussion, the author goes to considerable length to explain the effectiveness for the adjunctive use of antibiotics in the periodontal treatment of smokers and to their credit also the lack of clinical relevance. There are three important points to be made here:
“The number of significant figures gives a hint of accuracy. For example, 98.2o has three significant figures and might be regarded as correct to within 0.05o (One should not count on this level of accuracy.) Therefore, in these ambiguous circumstances, the author should tell what degree of accuracy is intended, as nearly as possible”(Mosteller 1992)
Links
Primary Paper
Assem, N.Z. et al., 2017. Antibiotic therapy as an adjunct to scaling and root planing in smokers: a systematic review and meta-analysis. Brazilian Oral Research, 31, pp.1–15. Available at: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-83242017000100951&lng=en&tlng=en.
Additional references
Dietrich, T. et al., 2015. Smoking, Smoking Cessation, and Risk of Tooth Loss: The EPIC-Potsdam Study. Journal of dental research, 94(10), pp.1369–75.
Keestra, J.A.J. et al., 2014. Non-surgical periodontal therapy with systemic antibiotics in patients with untreated chronic periodontitis: A systematic review and meta-analysis. Journal of Periodontal Research, (32), pp.689–706.
Lim, S.S. et al., 2012. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), pp.2224–2260.
Mosteller, F., 1992. Writing about numbers. In Medical uses of statistics. Boston: NEJM Books, pp. 375–89.
Rabelo, C.C. et al., 2015. Systemic antibiotics in the treatment of aggressive periodontitis. A systematic review and a Bayesian Network meta-analysis. Journal of Clinical Periodontology, 42(7), pp.647–657.
Zeng, J. et al., 2014. Reexamining the Association Between Smoking and Periodontitis in the Dunedin Study With an Enhanced Analytical Approach. Journal of Periodontology, 85(10), pp.1390–1397. Available at: http://dx.doi.org/10.1902/jop.2014.130577.
 Immediate placement of dental implants into fresh extraction sockets has for some time been an established surgical technique. The theory is that it preserves alveolar ridge, reduces morbidity, and is more acceptable to the patient. However, there may also be disadvantages such as reduced implant survival, unfavourable changes in the hard/soft tissue and extended treatment times. To standardise the type of implant placement they have been classified into four types:
Immediate placement of dental implants into fresh extraction sockets has for some time been an established surgical technique. The theory is that it preserves alveolar ridge, reduces morbidity, and is more acceptable to the patient. However, there may also be disadvantages such as reduced implant survival, unfavourable changes in the hard/soft tissue and extended treatment times. To standardise the type of implant placement they have been classified into four types:
The research question for this systematic review and meta-analysis was: ‘‘Do immediately inserted implants perform similarly to implants that are inserted into a healed socket?’’
This review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and registered with PROSPERO.
The population (P) was patients who had undergone osseointegrated implant insertion into fresh extraction sockets (I) or healed sockets (C). The primary outcome (O) evaluated was implant survival rate. Marginal bone loss, primary implant stability, and soft tissue changes were considered secondary outcomes. The following inclusion criteria were applied: Randomised controlled or prospective studies in English. More than five implants per group with a minimum of six months follow-up. Exclusion criteria were animal and in vitro studies, simple evaluations without comparators or analyses of loading protocols.
Two researchers independently selected and screened articles PubMed/Medline, Embase, and Cochrane databases and manually searched relevant specialist journals. Quality assessment was undertaken using the Jadad scale and Cochrane Collaboration’s tool for assessing risk of bias.
| Relative risk(95% Confidence Interval) | Probability | |
| Survival favours healed sockets | 2.49, (1.44 – 4.29) | p = 0.001 |
| Type 1 compared with type 2 | 1.45, (0.53 – 3.98). | p = 0.47 |
| Type 1 compared with type 3 | 5.25, (1.67 – 16.49) | p = 0.005 |
| Type 1 compared with type 4 | 2.86, (1.22 – 6.70) | p = 0.02 |
The authors concluded:-
In conclusion, immediate implant insertion should be performed with caution because implant survival rates are significantly lower than with implants inserted into healed sockets.
My intuition tells me that the authors may have the right answer but the evidence they present does not support this for various methodological reasons. The major problem is that the survival data is of relatively short duration and heterogeneous with a mean follow-up being 24 months, median 18 months and a mode of 12 months.
Clinicians mostly will only be interested in long-term data (60 months plus). Focusing on just these longer-term studies papers in the review just leaves three papers (Cooper et al 2014, Polizzi et al 2000 and Raes et al 2016) , so a second Raes paper (Raes et al 2013) with a stated 52 months follow up and the 2015 Oxby paper with 55 months follow up were reviewed and meta-analysed.
Looking at these research papers with the longest follow-up is simpler to appraise than the 30 the authors included. Full texts were obtained and the following conclusions made:
The 2013 Raes paper was therefore excluded as the follow-up was too short, and the Oxby paper as a retrospective study (exclusion criteria). The remaining studies were included in a meta-analysis. Group a. is the data as published in the systematic review and Group b. where LTF is considered in the calculations as a failure.
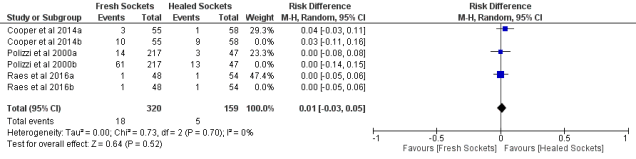
Fig.1 shows the new risk ratio (RR) for the long-term data has reduced from 2.49 to 1.28. If missing data is considered as a failure the RR drops to 1.06 (Fig. 2). An interesting observation is that the risk difference for Group a (Fig. 3) is 0.01.
Fig. 1. Forest plot for the event ‘60-month implants survival rates’ for Group a.
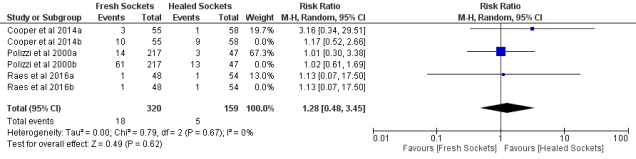
Fig. 2. Forest plot for the event ‘60-month implants survival rates’ for Group b.

Fig. 3. Forest plot for the Risk Difference ‘60 month implants survival rates’ for Group a.
In conclusion from this data there is no difference between techniques, possibly due to the ability to select cases rather than a true randomisation. One interesting point is that long-term survival for fresh v. healed was 94.4 and 96.9; if missing data is considered a failure 5-year survival drops by a further 15%. As usual the truth lies somewhere in between.
Mello CC, Lemos CAA, Verri FR, Dos Santos DM, Goiato MC, Pellizzer EP.Immediate implant placement into fresh extraction sockets versus delayed implants into healed sockets: A systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2017 May 3. pii: S0901-5027(17)31361-9. doi: 10.1016/j.ijom.2017.03.016. [Epub ahead of print] Review. PubMed PMID: 28478869.
Cooper LF, Reside GJ, Raes F, Garriga JS, Tarrida LG, Wiltfang J, Kern M, De Bruyn H. Immediate provisionalization of dental implants placed in healed alveolar ridges and extraction sockets: a 5-year prospective evaluation. Int J Oral Maxillofac Implants. 2014 May-Jun;29(3):709-17.
Polizzi G, Grunder U, Goené R, Hatano N, Henry P, Jackson WJ, Kawamura K, Renouard F, Rosenberg R, Triplett G, Werbitt M, Lithner B. Immediate and delayed implant placement into extraction sockets: a 5-year report. Clin Implant Dent Relat Res. 2000;2(2):93-9.
Raes S, Raes F, Cooper L, Giner Tarrida L, Vervaeke S, Cosyn J, De Bruyn H. Oral health-related quality of life changes after placement of immediately loaded single implants in healed alveolar ridges or extraction sockets: a 5-year prospective follow-up study. Clin Oral Implants Res. 2017 Jun;28(6):662-667. Epub 2016 May 22.
Oxby G, Oxby F, Oxby J, Saltvik T, Nilsson P. Early Loading of Fluoridated Implants Placed in Fresh Extraction Sockets and Healed Bone: A 3- to 5-Year Clinical and Radiographic Follow-Up Study of 39 Consecutive Patients. Clin Implant Dent Relat Res. 2015 Oct;17(5):898-907.
Raes F, Cosyn J, De Bruyn H. Clinical, aesthetic, and patient-related outcome of immediately loaded single implants in the anterior maxilla: a prospective study in extraction sockets, healed ridges, and grafted sites. Clin Implant Dent Relat Res. 2013 Dec;15(6):819-35.
Dental Elf – 2 August 2017
Dental Elf -12th Dec 2014