As the profession starts planning its phased return to clinical work in dental practice I thought it would be a good time to look through the updated ‘COVID-19: personal protective equipment use for aerosol generating procedures (AGPs)’ from Public Health England (PHE, 2020), and I became immediately confused as I referred back to my oral surgery training. Which comes first, the mask or the gown? It was quite challenging to find any recent primary research papers on surgical donning protocols so I have referenced a recent protocol from the NHS Foundation Trust (Newcastle_Hospitals, 2017). The two protocols are presented below (See Table 1.).
| Public Health England
donning instructions for AGPs |
Newcastle upon Tyne Hospitals standard surgical protocol |
| 1. Remove jewellery | 1. Remove jewellery |
| 2. Tie hair back | 2. Tie hair back + disposable surgical cap |
| 3. Hand hygiene | 3. Respirator/surgical mask |
| 4. Gown | 4. Eye protection/visor |
| 5. Respirator | 5. Hand hygiene |
| 6. Eye protection/visor | 6. Gown |
| 7. Gloves | 7. Gloves |
Table 1. Comparative donning protocols
The protocols diverge after Stage 2 where the standard surgical protocol involves wearing a surgical cap to prevent the possible contamination of the sterile field by falling hair, but also to prevent contamination of the hair during AGP’s/surgery. The protocol then goes, respirator/surgical mask, eye protection, hand hygiene, gown, and finally gloves. This process reduces the risk of cross contamination of the hands, gown, and gloves prior to treatment. The PHE guidance flips the protocol around where the hands are washed, then the gown, respirator, eye protection, and finally gloves are donned. The contentious area is that if the PPE following the PHE protocol needs to be replaced for the next patient there is an increased risk of cross contamination from the clinicians hands as they have now touched the head, face, ears and gown prior to gloving , this could be reduced in the standard surgical protocol. It would appear that the PHE guidelines are possibly based on an American Centre for Disease Control document from 2007(CDC, 2007) regarding ‘isolation precautions for preventing transmission of infectious agents in healthcare settings’ which then evolved into their ‘PPE guidelines for coronavirus disease’ (CDC, 2020). These guidelines were developed for treating patients in isolation wards where the number of actively infected individuals would be close to 100% (WHO, 2020) rendering cross contamination negligible as all the patients already have the disease.
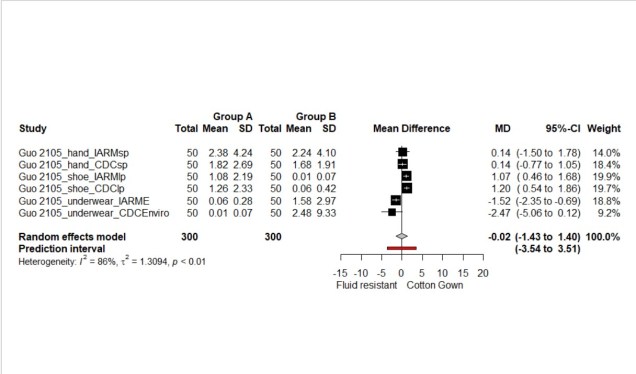
At present there is a high degree of uncertainty over the prevalence of infected/recovered individuals in the population who could attend a dental surgery for treatment, this uncertainty increases the possibility of cross infection via the sessional use of PPE if an asymptomatic patient should attend for treatment. This also holds true if the PPE is going to be changed between AGPs as there is also a risk of cross contamination of the new PPE, wearer, and surgery environment if doffing and re-donning is not performed perfectly. In a study by Phan and co-workers they found that 11% of scrub samples, and 7% of face samples were positive for respiratory virus after doffing (Phan et al., 2019b), and overall 90% of observed doffing was incorrect (Phan et al., 2019a). As a precautionary principle perhaps these small but important changes in the donning of PPE should be considered; mask, visor, hand hygiene, then gown and gloves. The concern here is not about maintaining sterility as in routine surgery but trying to avoid virus transfer to the new PPE while we await more data on the risk posed by AGPs of dental origin to both the patients and the dental team.
Disclaimer: The article has not been peer-reviewed; it should not replace individual clinical judgement, and the sources cited should be checked. The views expressed in this commentary represent the views of the author and not necessarily those of the host institution. The views are not a substitute for professional advice.
References
NEWCASTLE_HOSPITALS. 2017. Surgical Scrub, Gown and Glove Procedure [Online]. The Newcastle upon Tyne Hospitals NHS Foundation Trust. Available: http://www.newcastle-hospitals.org.uk/downloads/policies/Infection%20Control/SurgicalScrubGownandGloveProceduresPolicy201706.pdf [Accessed].
PHE.2020. PHE COVID-19 Donning quick guide gown version [Online]. Public Health England. Available: https://www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures [Accessed].
CDC. 2007. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007) [Online]. Available: https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html [Accessed].
CDC.2020. Using Personal Protective Equipment (PPE) [Online]. Available: https://www.cdc.gov/coronavirus/2019-ncov/hcp/using-ppe.html [Accessed].
PHAN, L. T., MAITA, D., MORTIZ, D. C., WEBER, R., FRITZEN-PEDICINI, C., BLEASDALE, S. C., JONES, R. M. & PROGRAM, C. P. E. 2019a. Personal protective equipment doffing practices of healthcare workers. Journal of occupational and environmental hygiene, 16, 575-581.
PHAN, L. T., SWEENEY, D., MAITA, D., MORITZ, D. C., BLEASDALE, S. C., JONES, R. M. & PROGRAM, C. D. C. P. E. 2019b. Respiratory viruses on personal protective equipment and bodies of healthcare workers. Infect Control Hosp Epidemiol, 40, 1356-1360.
PHE. 2020. PHE COVID-19 Donning quick guide gown version [Online]. Public Health England. Available: https://www.gov.uk/government/publications/covid-19-personal-protective-equipment-use-for-aerosol-generating-procedures [Accessed].
WHO 2020. Rational use of personal protective equipment for coronavirus disease (COVID-19): interim guidance, 27 February 2020. World Health Organization.